
It’s almost the end of World Immunization Week and it’s the current climate its now more than ever important to celebrate the successes of immunization programs. I personally have also been working in the field of infectious diseases and vaccines for 20 years, and I’ve never stopped loving working in this space – from working in a lab and mouse models on new vaccine candidates to clinical trials to immunisation practice and policy; and outbreak response.
So this year as we reflect on World Immunization Week, I am delighted to share the work of my team who is working towards finding solutions to addressing immunisation inequities and monitoring systems.
Making Vaccines Work: How Better Data and Stronger Systems Improve Immunisation Equity
At the Infectious Diseases, Immunisation, and Emergencies (IDIE) team, we believe that making vaccines is just the start. The real challenge is making sure everyone — no matter where they live or who they are — has reliable and equal access to vaccines. It requires good policies and practices, supported by data, systems, and a strong workforce.
Our work brings together different aspects of immunisation program together. We develop innovative solutions to support programmatic interventions, disease surveillance, and emergency (e.g. outbreaks) preparedness and responses. All of this work is backed by engagement and capacity building.
Read about some of our project successes in the last year

Electronic immunisation registers (EIRs) are information systems used to capture, store, access and share individual-level data on vaccine doses administered, and can strengthen decision-making about immunisation. We conducted an evaluation of the Lao PDR EIR, implemented first in 2022, to identify opportunities to improve its implementation, scale-up and sustainability. We used a mixed method approach to examine user perspectives about the EIR, experiences with implementing the EIR, and its potential benefits. We collected data through a desktop review, survey of healthcare workers, observation of workflow, key informant interviews with decision-makers, and an analysis of data quality in the EIR. We found high levels of enthusiasm for the EIR and its future among both healthcare workers and those involved at a health systems level. Participants discussed that data collection using the EIR was working well, but that data use was still limited. Participants cited a number of factors constraining the EIR from achieving its full potential including lack of capacity and capability among the health workforce, a lack of policies and formal regulations, perceived limited ownership by the government, lack of clarity on future sources of funding and digital infrastructure constraints.
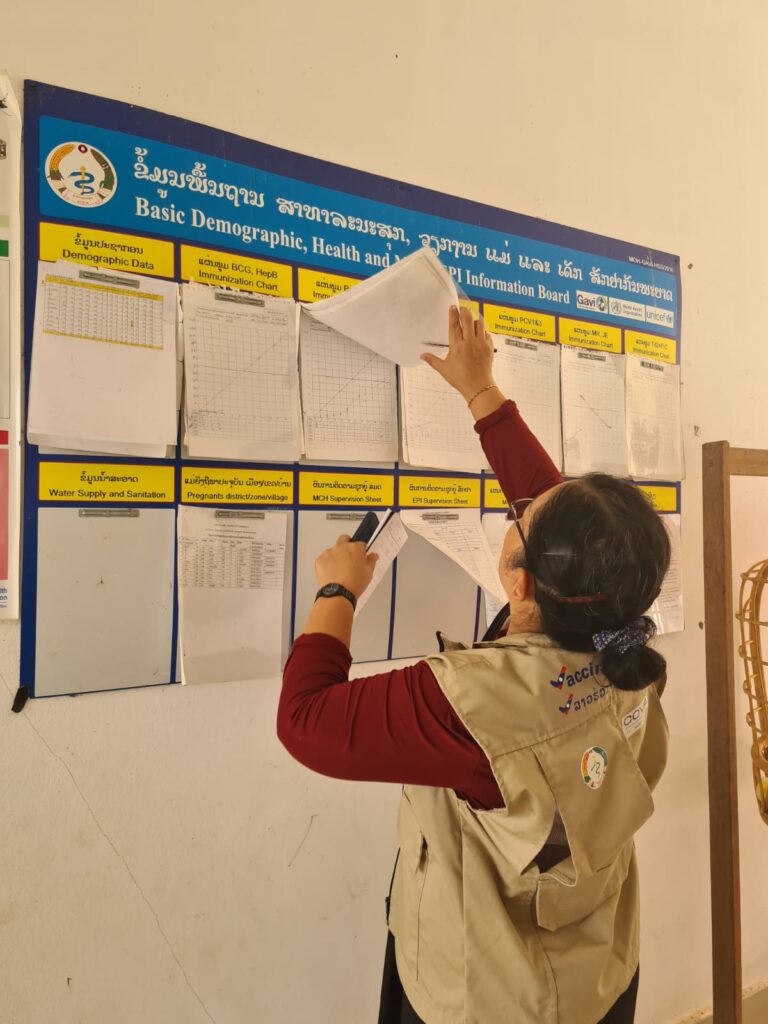
Our team has acquired another grant to continue our work on improving the Lao PDR EIR. In this continuation of this body of work, we will use a pre-post study design to examine the role of the EIR in improving vaccine uptake in Lao PDR. We will examine the effects of implementing a package of interventions, including increasing the capability and use of EIRs among healthcare workers, embedding a national vaccine data officer within the Ministry of Health, and introducing EIR-linked alerts.
We are in the process of publication! Stay tuned for our papers
Measuring the status of immunisation for children living with disability in Fiji

Measuring the status of immunisation for children living with disability in Fiji highlights the critical issue of limited data on immunisation coverage among children with disabilities in low- and middle-income countries (LMIC), including Fiji where these children face significant inequities in access to vaccines. This project aims to measure vaccination status in children with disability in Suva-Nausori corridor, Fiji and understand the social and behavioural drivers for vaccination. It found that while Fiji demonstrates strong overall immunisation rates, the specific coverage for children with disabilities remains largely unknown, underscoring a gap that needs urgent attention. Notably, vaccination coverage for all National Immunisation Programme vaccines is significantly lower among adolescents aged 15-19 years, with only 55.1% fully vaccinated against basic vaccines. This statistic emphasises the need for targeted interventions to ensure equitable immunisation for all children, particularly those with disabilities, to protect their health and well-being.

Following on from our previous work, our team have acquired another grant to fund work to improve vaccine uptake in children with disability aged 2-19 years in Fiji. We specifically aim to co-design and develop a package of interventions to improve vaccination in children with disability with family and service providers; implement key vaccine-related strategies in under and un-vaccinated children with disability within the existing health, education, and disability systems; develop a core set of tools that can be used to identify drivers for under-vaccination design tailored interventions to improve vaccination in children with disability in the Pacific.
Sustaining demand for the Essential Programme on Immunization in Low-and-Middle-Income Countries
This project activity aims to help understand how the COVID-19 pandemic affected demand for childhood and adolescent vaccines provided under the Essential Programme on Immunization. It will identify which factors are associated with ‘resilient demand’, i.e. what factors explain why some countries were able to sustain demand and high coverage of these vaccines over the course of the COVID-19 pandemic, while other countries experienced declines.
Read our paper here, and stay tuned for upcoming papers
Training and capacity building of immunisation health workforce in Southeast Asia
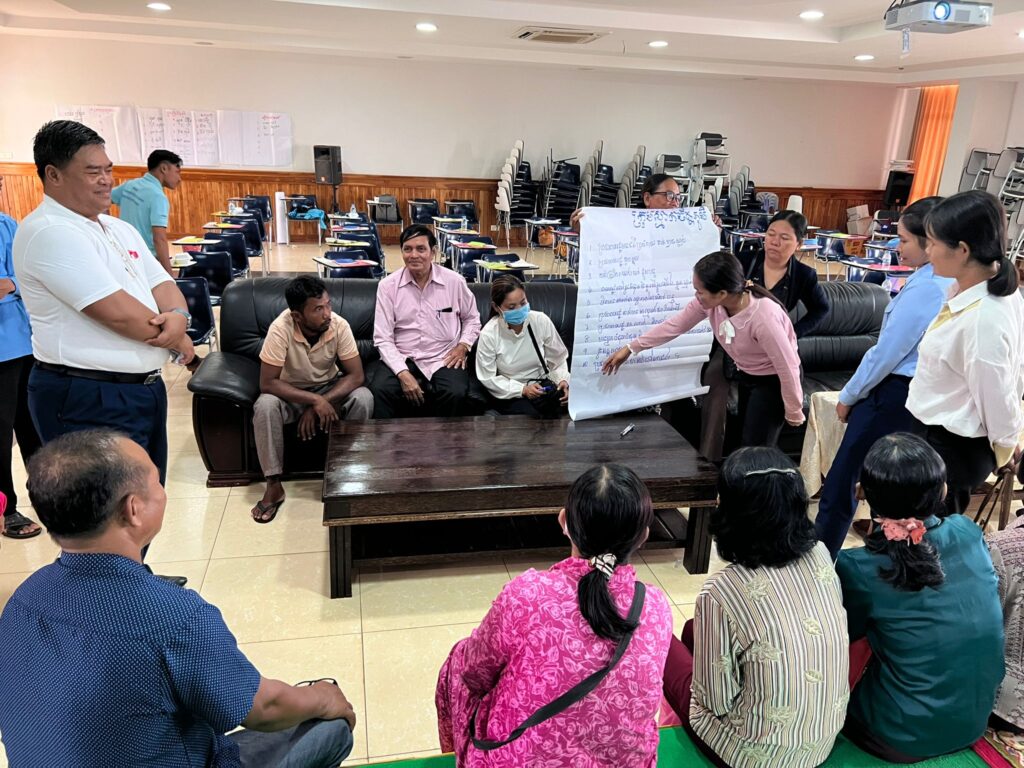
Our team designed and delivered training for the health workforce involved in delivery of routine and COVID-19 vaccination in Cambodia and Lao PDR. The programme was developed and delivered by the project team in partnership with local stakeholders and technical experts. We trained 445 participants from professional groups across various levels and sectors of the health system. This examination of the successes and challenges of immunisation training programme implementation in Southeast Asia can support the development and evaluation of future impactful and sustainable learning and performance management initiatives in the region.
Read our paper here:
Pro-equity strategies to improve vaccination uptake, coverage and timeliness among priority groups that are unvaccinated: A systematic review
This review looked at how to improve vaccination for people who often miss out—like those living in rural areas, migrants, ethnic minorities, and people with disabilities. It found that community outreach, mobile clinics, and better reminder systems helped increase coverage, especially in rural settings. However, strategies were mostly tested in richer countries, were small-scale, and rarely built into the regular health system. Groups like migrants and people with disabilities were often overlooked. To really make vaccination more fair, we need more long-term programs, better data on who’s being reached, and stronger efforts to embed equity into everyday health services.
Improving immunisation systems through data for decision-making in Pacific Island Countries

Health information systems are considered the bedrock of health systems as they produce vital data necessary for public health decision-making. For immunisation, having accurate, timely data on vaccination coverage is crucial to inform strategic and programmatic decisions about immunisation programs and achieve high, equitable coverage. While countries invest substantial resources in collecting and reporting vaccination coverage data, their use in decision-making remains limited. In my PhD thesis, I examine the role of data for decision-making in strengthening immunisation systems in Pacific Island Countries and Territories (PICs). This work first explores how immunisation system performance is measured, and examines the relationships between immunisation performance in routine and emergency settings in small island developing states. It then examines what immunisation data are most useful to decision-makers in PICs. Finally, it examines how data is used for decision-making about immunisation in the Pacific, and the role of digital technologies (like electronic immunisation registers) in enabling data-driven decision-making. This PhD is supervised by A/Prof Meru Sheel, Prof Martyn Kirk, Dr Ginny Sargent, Dr Akeem Ali.
Read some of our study outputs here:
Exploring the role of religious leaders in routine immunisation in Indonesia
Indonesia’s diverse cultural and religious landscape features influential religious leaders who hold revered positions, affecting not only spiritual matters, but also social domains including healthcare decisions. The interaction between religion and vaccination has gained prominence in Indonesia, with a fatwa (a religious ruling) on the permissibility of measles vaccination in 2016 affecting vaccination acceptance, particularly among Muslim Indonesians. Religious leaders have the potential to influence attitudes toward immunisation, affecting vaccination rates, and ultimately, disease control. While studies have explored the roles of religious leaders in specific vaccination programs in Indonesia, comprehensive research on routine immunisation is lacking, especially regarding leaders of other faiths. This study aims to explore religious leaders’ views on routine immunisation, assess their involvement in routine immunisation, and recommend strategies for better integration of their role in these programs. This PhD is supervised by Prof Julie Leask, A/Prof Meru Sheel, and Dr Suryo Bagas Bintoro
Effectiveness and cost-effectiveness of measles vaccination strategies for children in low income settings
This project focuses on optimising measles vaccination programs for children under five in Ethiopia by assessing their impact and cost-effectiveness. It begins with an analysis of measles surveillance data to understand trends in disease incidence and vaccination coverage. Using a compartmental infectious disease model, the project simulates different vaccination scenarios to estimate future health outcomes. An economic evaluation will compare the costs and benefits of each strategy, while qualitative methods will explore the on-the-ground challenges and successes of implementation. Together, these approaches aim to inform practical, evidence-based recommendations to strengthen measles control efforts and improve child health outcomes. This PhD is supervised by Prof Andrew Hayen, A/Prof Meru Sheel, A/Prof Jane Frawley, and Dr Abela Mahimbo.
Read some of our study outputs here:
Interested in learning more about what we do? Learn more about our research projects and see a full list of our papers here



